
Cervical Cancer
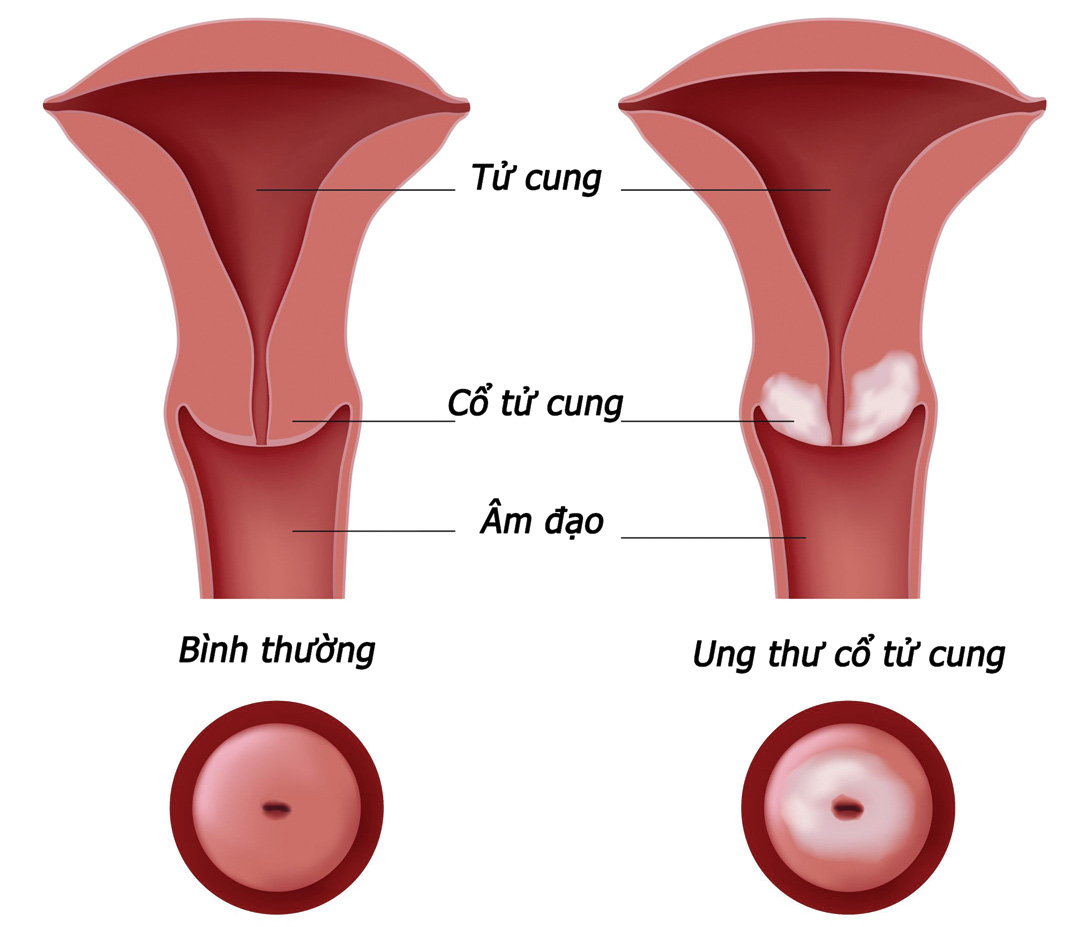
WHAT IS CERVICAL CANCER?
Cervical cancer is the fourth most common cancer after breast, colorectal and lung cancers. In 2018, there were approximately 570,000 new cases of cervical cancer and 311,000 deaths worldwide.
The main cause of cervical cancer is infection with the human papillomavirus (HPV). It is one of the most common sexually transmitted infections. HPV causes genital warts, cervical ectropion, and cervical cancer. When an infection caused by HPV is left untreated, the uncontrolled growth of abnormal cells can become cancerous. It usually takes about 10 to 15 years for a persistent HPV infection to progress to cancer. Therefore, HPV testing is important for early diagnosis of cervical cancer.
SIGNS OF CERVICAL CANCER
Cervical cancer usually develops insidiously over a long period of time (it takes several years). During this time, cells in the cervix will change abnormally due to a change in the vaginal environment or infection with the HPV virus. The deformation of these cells that occurs before cancer appears is called dysplasia or cervical intraepithelial neoplasia (CIN).
The first sign of cervical cancer is abnormal vaginal bleeding, such as bleeding between menstrual periods, longer than normal periods, bleeding after or during menstruation. relationship. Signs of developing cancer may include pelvic pain, abnormal urination, and leg swelling. If the cancer has spread to nearby organs or lymph nodes, tumors can affect the way those organs work, for example the tumor is pressing on the bladder or blocking a vein.
ETIOLOGY
Infection with the human papillomavirus (HPV) is the most common cause or risk factor for cervical cancer. These viruses are transmitted through oral, vaginal, or anal sex.
All sexually active women are at risk for cervical cancer. However, women who have sex with many people, having sex early in life or with out protect have a greater risk of contracting the disease.
HPV can cause cervical cancer.
- Low-risk HPV types: can cause genital warts or very small cell changes in the cervix. Low-risk HPV types include: HPV 6, 11, 40, 42, 43, 44, 53, 54, 61, 72, 73, and 81. HPV types 6 and 11 are involved in about 90% of acne cases. genital toad.
- High-risk HPV types that cause cervical cancer: can cause abnormal cells to form in the cervix. These abnormal cell changes can gradually develop into cervical cancer if not removed. High-risk HPV types include: HPV 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 68. In which, HPV 16 and 18 are the most dangerous, because they cause about 70% of cervical cancers.
.jpg)
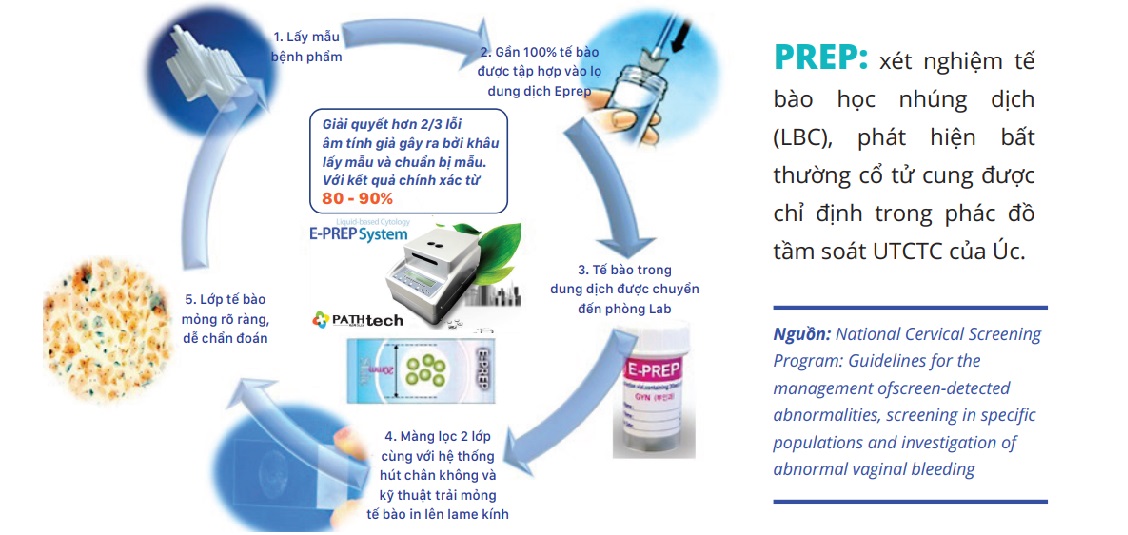
Cervical cancer screening
To screen for cervical cancer most effectively, it is necessary to combine two methods: PAP (E-Prep) and HPV-DNA (GenHPV). Specifically:
- For the Pap (E - Prep) test, the sample is checked for the presence of any abnormal cells. E - Prep results will indicate whether the cells in the cervix are damaged, to what extent.
- For the GenHPV test, the sample is checked for the presence of strains of HPV.
Due to their specific tasks, but these two methods are not interchangeable, they complement each other to help doctors diagnose and provide appropriate treatment for each individual patient.
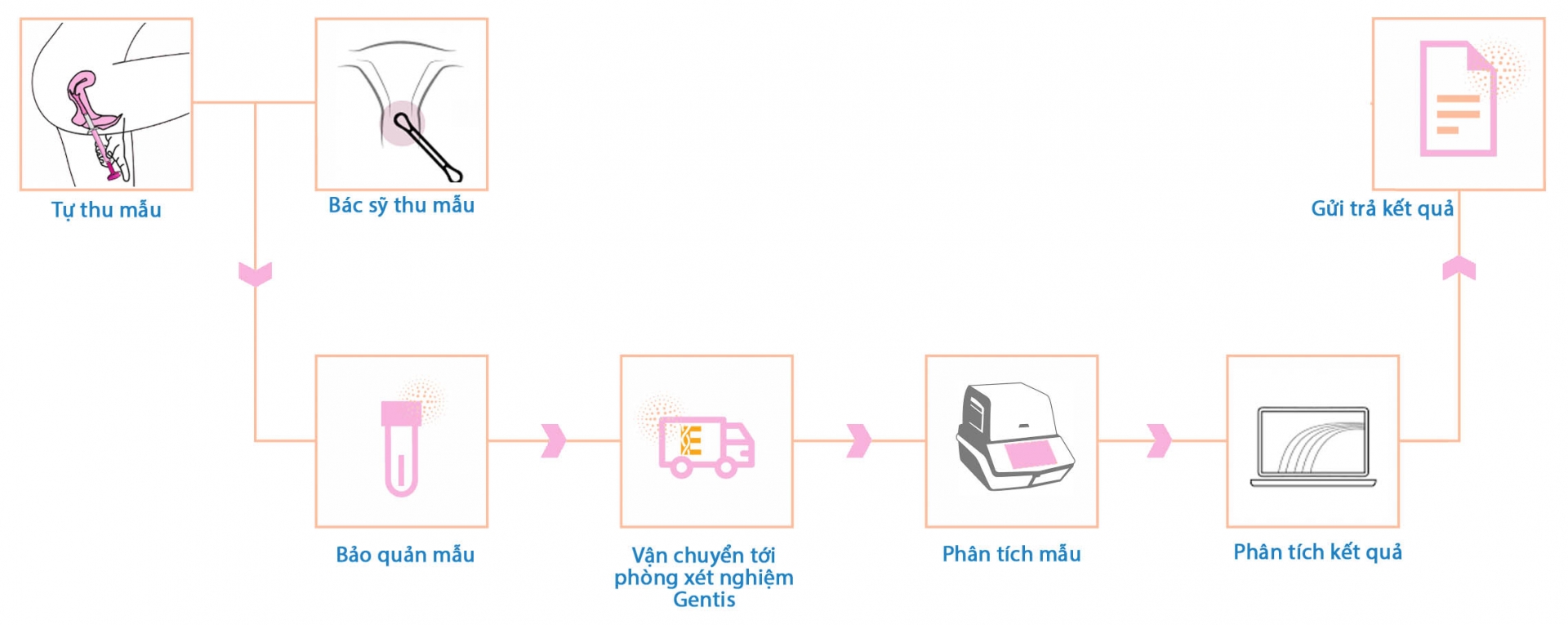
TESTING AT GENTIS
GenHPV testing procedure at GENTIS
E-Prep Testing Procedure
Specimens (cervical smear) will be placed in a vial of Eprep solution to remove impurities (blood, mucus, etc.) by double membrane technology and a vacuum system that smears a thin layer of cells on the slide.
GENHPV SCREENING TEST IN GENTIS
Sample type: Self-collected cervical smear using Evalyn instrument - Netherlands
Time to return results: from 2 days
.jpg)
=> Call 1800 2010 for advice and order a home delivery sample collection.
Please fill in the information below to receive our supports and consultations!







